Cortisol: The Primary Stress Hormone
When the body becomes stressed, the Sympathetic Nervous System (SNS) activates what is known as the "fight or flight" response. As a coping mechanism, the body shifts its energy resources toward either fighting off a life threat or fleeing from the enemy. The SNS signals the adrenal glands to release hormones called adrenalin (epinephrine) and cortisol. This in turn suppresses the Parasympathetic Nervous System (PSNS) as the two opposing systems cannot operate simultaneously.
Stress: acute or chronic?
Stress can be classified into two main types: acute stress and chronic stress. Acute stress is the immediate reaction to a threatening situation. Once the threat has passed, our stress hormones return to normal levels with no long-lasting effects.
Chronic stress, on the other hand, is ongoing stress that often isn’t triggered by danger or a life-threatening situation, it can be the low-lying daily stressors of diet, lifestyle, work or relationships that never resolve and continue to place a strain on your emotional wellbeing. Chronic stress means that there is a constant production of cortisol creating damage, inflammation and wear and tear on the body as it is unable to find a calm balance. The body tries to maintain equilibrium at every moment; however, it is unable to do this when faced with high cortisol levels.
Continuing high cortisol levels will eventually result in physical health problems such as digestive issues, general inflammation, weight gain, hormone imbalances, heart disease and diabetes.

How high cortisol levels affect the whole body
Why is high cortisol production a problem? In a nutshell, the theory is that with our ever-stressed, fast-paced lifestyle, our bodies are pumping out cortisol almost constantly and this can wreak havoc on our general health.
Blood Sugar Imbalance and Diabetes
Under stressful conditions, cortisol provides the body with glucose by tapping into protein stores via a process called gluconeogenesis in the liver. This energy can help an individual fight or flee a stressor. However, elevated cortisol over the long term consistently produces glucose, leading to increased blood sugar levels (increasing the risk of type 2 diabetes or insulin resistance).
Weight Gain and Obesity
Repeated elevation of cortisol can lead to weight gain due to body fat stored along the abdomen and surrounding our vital organs. Cortisol can mobilize triglycerides from storage and relocate them to visceral fat cells (those under the muscle, deep in the abdomen). Also, visceral fat cells have more cortisol receptors than subcutaneous fat – hence, weight gain during hormonal changes (puberty, perimenopause) and long-term stressful situations.
A second way in which cortisol may be involved in weight gain goes back to the blood sugar-insulin problem. Consistently high blood glucose levels along with insulin suppression lead to cells that are starved of glucose. Those cells are crying out for energy and one way to regulate is to send hunger signals to the brain. This can lead to overeating and we all know that unused glucose is eventually stored as body fat.
Another connection is cortisol’s effect on appetite and cravings for high-calorie foods. Cortisol may directly influence appetite and cravings by binding to hypothalamus receptors in the brain. Cortisol also indirectly influences appetite by modulating other hormones and stress responsive factors known to stimulate appetite.
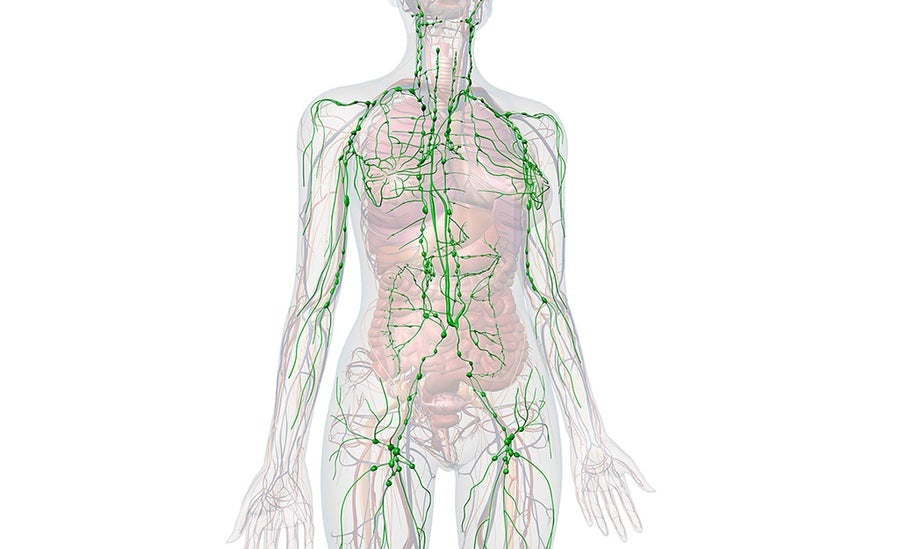
Immune System Suppression
Cortisol functions to reduce inflammation in the body, which is basically good. Over time, however, these efforts to reduce inflammation also suppress the immune system. Chronic inflammation caused by lifestyle factors such as poor diet and stress will keep cortisol levels soaring, wreaking havoc on the immune system and causing inflammation in the long term.
Gastrointestinal Problems
Cortisol activates the SNS and depresses the PSNS (rest and digest action). The PSNS is stimulated during quiet activities such as eating, which is important because enzymes and hormones controlling digestion and absorption must be working at their peak levels for the body to best use food energy. Long term suppression of digestive activity can compromise proper digestion and absorption. This leads to indigestion which causes the mucosal lining to become irritated and inflamed. Problems like ulcers, colitis, reflux and IBS can then develop. Sounds familiar?
Cardiovascular Disease
Cortisol constricts blood vessels and increases blood pressure to enhance the delivery of oxygenated blood. Over time, such arterial constriction and high blood pressure can lead to vessel damage and plaque buildup—the perfect scenario for a heart attack. This may explain why stressed-out type A personalities are at significantly greater risk for heart disease than the more relaxed type B personalities.
Fertility Problems
Elevated cortisol relating to prolonged stress can lend itself to erectile dysfunction or the disruption of normal ovulation and menstrual cycles. Furthermore, the androgenic sex hormones are produced in the same glands as cortisol and epinephrine, so excess cortisol production may hamper optimal production of these sex hormones. Check out our article on the top 10 fertility foods.
Other Issues
Long-term stress and elevated cortisol may also be linked to insomnia, chronic fatigue syndrome, thyroid disorders, dementia, depression, and other conditions.
How to de-stress for optimal health
The Anti-Inflammatory Diet
Systemic inflammation, as noted previously, causes elevated cortisol levels. If we can naturally decrease inflammation in the body and minimize stress, decreased cortisol levels should follow, resulting in decreased chronic disease risk and improved wellness. Incidentally, dietary strategies for controlling inflammation may also help with adrenal support in general, since diet can directly affect adrenal burden (e.g. cortisol is released in response to metabolic demands).
To minimize inflammation and thereby cortisol levels, the following are recommended:
- a low glycemic load diet
- elimination of trans fats and minimal intake of saturated fats
- elimination or reduction in consumption of caffeine and alcohol
- increasing consumption of whole plant foods to maximize intake of fiber, antioxidants, and phytonutrients (vegetables, fruits, whole intact grains, nuts, seeds, and beans)
- meeting recommended intake of omega-3 fatty acids
- regular exercise, breath work and meditation practices
- address psychological/ emotional issues preventing a calm nervous system (stress management)
- ensuring quality and more sleep
- following the Happy Hormones 8-Week Program
Summary
Implementation of targeted dietary and lifestyle approaches is an extremely powerful way to reduce stress, minimize inflammation, and lower your risk for illness and chronic disease. True, the many biochemical processes involving cortisol and other hormones, stress, and inflammation and their impact on health and disease risk are complex and elaborate. The therapeutic diet and lifestyle strategies, however, are not. The more we learn about the extraordinary healing power of the body and the way it responds to the demands placed on it, the more we will value good health.
REFERENCES
Chiodini et al. Cortisol Secretion in Patients With Type 2 Diabetes: Relationship with chronic complications. Diabetes Care. 2007 Jan; 30(1): 83-88.
https://doi.org/10.2337/dc06-1267
Rooney KL and Domar AD. The relationship between stress and infertility. Dialogues in Clinical Neuroscience. 2018 Mar; 20(1): 41–47.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016043/
Carvalho et al. Does the Mediterranean Diet Protect against Stress-Induced Inflammatory Activation in European Adolescents? The HELENA Study. Nutrients. 2018 Nov; 10(11): 1770.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6266959/
Harvard Health Publishing. Why stress causes people to overeat. Harvard Mental Health Letter. 2012 January.
https://www.health.harvard.edu/staying-healthy/why-stress-causes-people-to-overeat