The Vaginal Microbiome
Just like our gut has a bacterial community of its own, so does our vagina! And when it comes to women’s health, this dynamic ecosystem of microorganisms becomes particularly important.
The vaginal microbiome can directly impact fertility, immunity and even libido.
Research shows that optimum sexual and reproductive health in women is associated with a vaginal microbiota dominated by a range of Lactobacilli species. Lactobacillus crispatus is often considered the dominant bacterial resident in an ideal environment, although a healthy vaginal microbiome should also be crowded with other species such as L. iners, L. jensenii and L. gasseri.
One important thing to note about the vaginal microbiota is that microbial diversity within this community can vary across different ethnic groups. So as with everything within the holistic health space, we shouldn’t be limited by generalised parameters; rather, we should expect different microbial presentations among women when it comes to the vaginal microbiome.
Why do we want a lactobacilli-dominated ecosystem within the vagina?
It has been observed that lactobacilli bacteria thriving in the human vaginal microbiome promotes a healthy environment which protects women against a vast range of opportunistic infections and sexually transmitted pathogens. Here are just a few benefits of a lactobacilli-dominated vaginal microbiota:
- Enhances fertility
- Reduces HIV transmission
- Reduces the risk of sexually transmitted infections (STIs)
- Prevents vulvovaginal atrophy (VVA)
- Protects against cervical cancer
- Promotes better birth outcomes
- Protects against vaginal dryness and urinary tract infections (UTIs)
What causes disruption to the vaginal microbiota?
Dysbiosis is the term used to refer to the disruption of the microbes within a microbial community. The condition predisposes a woman to a range of gynaecological and urogenital conditions such as aerobic vaginitis (AV), bacterial vaginosis (BV), pelvic inflammatory disease, sexually transmitted diseases (STDs), and even premature birth. Both physiological and lifestyle factors can bring about this disruption in the proportion of bacteria. Here are just a few examples:
- Oral antibiotic use (Yes, you read right – antibiotics cause damage to more than just your gut!)
- Spermicide use
- Excessive douching and vaginal washing (especially with chemical-based feminine washes)
- Multiple sexual partners
- Increased frequency of intercourse
- Post-menopause hormonal changes
- Smoking
What can we do to nurture the vaginal microbiota?
Just like the gut, we want to limit chemical exposure to strengthen and enhance the bacterial colonies in the vagina. There is a range of different day-to-day practices that you can apply to further support and even enhance vaginal health.
Something as simple as not over-washing can actually promote a healthier microbial community in the vagina. You see, the bacterial colony in this area is a powerhouse tribe that has its own self-cleaning system. So the less we disrupt this process, the better. I recommend leaving your washing to other areas of the body and not using soaps and washes down below!
Another helpful tip is opting for bamboo or organic cotton underwear. They’re amazingly breathable and have lower levels of toxicity that will certainly have a positive impact on the vaginal microbiota. The same goes for sanitary products like toilet paper, wipes, and menstrual pads – go organic whenever possible as less exposure to toxins is quite vital for such an intimate section of your body.
Using a good quality organic lubricant during intercourse is also a good idea for those who experience vaginal dryness. I know of some women who’ve used coconut oil as an alternative but let me tell you it isn’t exactly a great option. For starters, our natural vaginal secretions are aqueous or water-based to facilitate easy elimination of dead cells and bacteria from this area of our body. An oil-based lubricant like coconut oil can alter vaginal pH as well as the antimicrobial effects acting on the happy bacteria and have a negative impact on the vaginal microbiome.
What should be done if there’s an imbalance in the vaginal microbiota?
First, it’s imperative that you address and test for a specific imbalance with the support of a practitioner. The practitioners in our online clinic can assist you with your specific concern. Determining the clear-cut difference between hormonal changes and bacterial imbalances within the vaginal microbiome is extremely vital as the lines can be a little blurred when it comes to this.
Lactulose
Lactobacilli in the vagina need nourishment in order to survive. Lactulose is the answer here as the prebiotic promotes the growth of symbiotic microflora and is most often utilised as a food source by those beautiful lactobacilli strains. The positive news is that lactulose cannot be utilised by pathogens like candida and is readily fermented to lactic acid within the vagina. This is crucial in lowering pH levels for a more favourable vaginal microbiota.
Lactulose comes in liquid form and is really simple to apply. An intravaginal application can consist of 2ml of lactulose syrup mixed well in 8ml of warm water and applied via syringe or spray before bed. Do this nightly for one week, then twice or thrice weekly for another three weeks to get maximum benefits.
Green Tea
Green tea is another potential vaginal prebiotic which has been shown to further encourage the growth of lactobacilli and inhibit pathogen growth. Additionally, green tea naturally decreases pH and also prevents the formation of biofilms which surround pathogenic bacteria strains for protection.
Incorporate this step for balancing vaginal microbiome by making a strong green tea using organic loose leaf. Let this steep until cool, add to a glass spray bottle and use as a vaginal spray. You could also add the lactulose formulation to this if you wish.
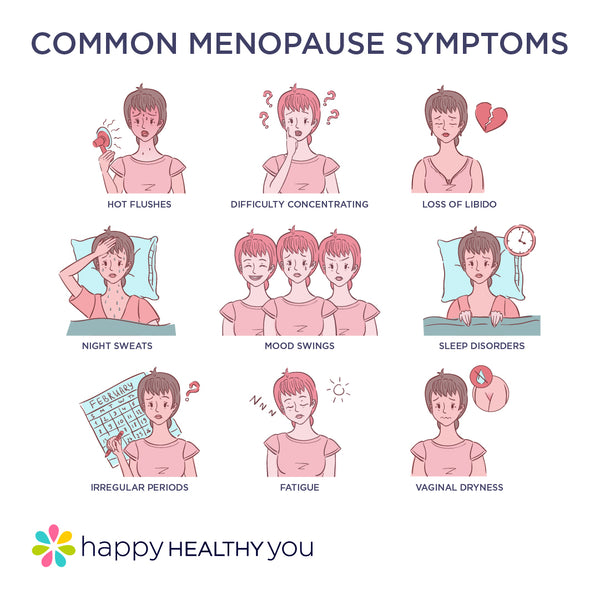
Menopause and the vaginal microbiome
It’s important to be aware that during and after menopause, oestrogen levels drop and so does the glycogen content within the vaginal epithelium. As a result, the lactobacilli count can also decline. With the fewer amounts of lactobacilli, we commonly see vaginal pH increase and this is where issues can arise. This can bring changes like vulvovaginal atrophy, vaginal dryness, and also impaired sexual health.
You need not worry, however. The practices I mentioned above will help keep things in check. Probiotic supplementation may also be necessary for this stage of your hormonal journey.
Optimum hormonal and reproductive health is our main goal here at Happy Healthy You. If you’re currently experiencing hormonal issues that might be preventing you from doing the things you love, I encourage you to take our FREE hormonal assessment so you can better understand your unique hormonal profile Our team of experienced naturopaths are ready to assist and help you manage and treat your symptoms!
Summary
For us women, the vaginal microbiome is an area of our health that should not be disregarded. It can enhance fertility outcomes, protect against infection and also optimise overall health and wellbeing. Keeping things simple with this area is important, so less is best! If you’re experiencing imbalances, it’s advisable to test and not just guess, so be sure to work with an Integrative Practitioner to assist you with this.
REFERENCES
Lewis, F et al. Vaginal Microbiome and its relationship to Behaviour, Sexual Health, and Sexually Transmitted Diseases. Obstetric Gynaecology. 2017;129(4): 643-654.
https://doi.org/10.1097/aog.0000000000001932
Barrientos-Duran, A et al. Reviewing the Composition of the Vaginal Microbiome; Inclusion of Nutrition and Probiotics Factors in the Maintenance of Eubiosis. Nutrients. 2020;12(2): 419.
https://doi.org/10.3390/nu12020419
Lokken, E et al. Impact of Preconception vaginal microbiota on womens risk of spontaneous preterm birth. Obstetrics and Gynaecology. 2020;10.
http://dx.doi.org/10.1136/bmjopen-2019-035186