Endometriosis: More Than Just a Hormonal Disease
While endometriosis may be affected by our hormones, it isn’t purely a hormonal and gynaecological disease. This means it affects far more than just your reproductive system and involves more than just your hormones. For this reason, we should have this in mind when considering treatment options.
Solely suppressing your cycle or cutting off your body's supply of estrogen in an attempt to 'quieten' lesions is a reductionist approach to treating endometriosis. The pill, hormone injections, or implanted devices can help relieve symptoms but they DO NOT tackle the whole beast.
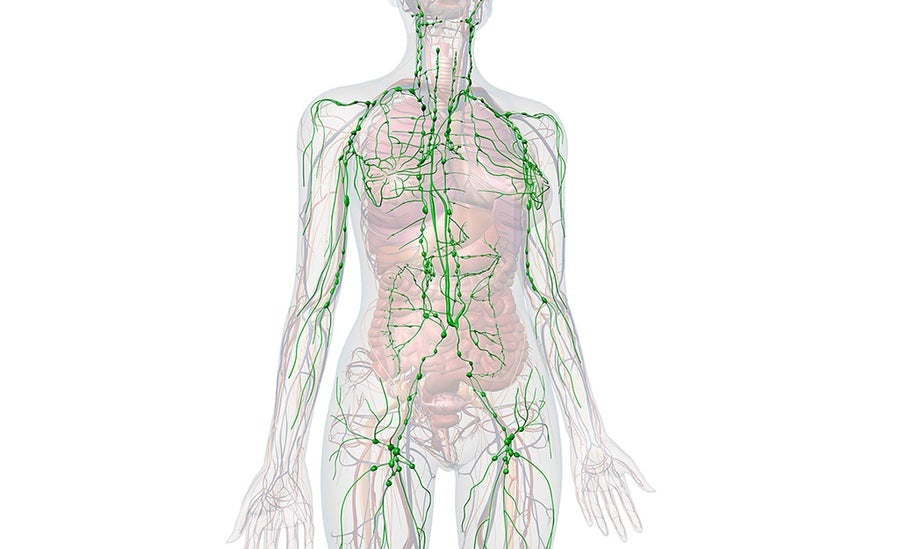
Endometriosis is a systemic, inflammatory, immunological, and hormonal disease.
Endometriosis involves inflammation of the whole body where multiple organ systems may be affected with lesions. There is activated immune activity in which immune cells fail to 'mop up' ectopic endometriosis cells. As a result, immune activity drives inflammation, lesion deposits and growth, free radical formation, and pain.
We are also seeing more prominent evidence of endometriosis behaving like a microbial disease. Women with endometriosis were observed to have contamination of bacterial toxins in menstrual blood and pelvic fluid. These toxins or lipopolysaccharides originate from specific gram-negative bacteria found in the pelvic cavity. These specific bacterial endotoxins are also hypothesised to play a role in the development and worsening of endometriosis. They release inflammatory mediators which further drive pain and inflammation.
Suboptimal gut health is a likely reason for the presence of the said bacteria in the pelvic cavity. Movement of bacteria from the digestive system to the reproductive system can occur in cases where there is a dysbiotic digestive tract. If you have endometriosis (or suspect you do) and you experience digestive symptoms, then you should address gut bacteria balance.
Key points to consider when looking beyond hormones and gynaecology
1. Remove trigger foods from your diet.
These may be more personal and specific depending on your sensitivities but generally speaking, eliminate anything containing gluten, dairy, refined sugar, processed and unfermented soy. We recommend doing this for at least three months.
2. Replenish your gut bacteria.
Eat plenty of high-fibre plant material and prebiotic foods. If you struggle with SIBO (small intestinal bacterial overgrowth), you may need to work with a practitioner one-on-one to eliminate the overgrowth. Begin to introduce some fermented foods and take a practitioner-grade probiotic.
3. Be mindful of histamine.
This can be prevalent in women with endometriosis. If you have a histamine sensitivity, it’s important to note that fermented foods and certain strains of probiotics are histamine-forming and should be consumed minimally until you naturally lower your histamine levels and your threshold increases. Some examples of histamine-friendly probiotic strains include Bifidobacterium infantis, Bifidobacterium bifidum, Bifidobacterium longum and Lactobacillus plantarum. These are soil-based probiotics so ensure that you are spending time in nature and walking barefoot.
4. Address the bacterial endotoxins which may be present.
Although this is a theory, albeit a strong one, you can try experimenting with herbal antimicrobials. The plant compound berberine has been studied in adenomyosis specifically and demonstrates the ability to inhibit adenomyosis proliferation driven by bacterial endotoxins.
5. Follow an anti-inflammatory diet and incorporate anti-inflammatory nutrients in your regime.
You need powerful free-radical scavengers to combat endometriosis. N-Acetyl Cysteine, a precursor to your body's most potent detoxifier and antioxidant, glutathione, has been shown to help shrink endometriosis lesions. Others to consider include zinc, curcumin (the active constituent in turmeric and Happy Turmeric), vitamins A, C, and E, ECGC (green tea extract), resveratrol and melatonin.
6. Look at ways to balance your overall endocrine system and boost natural progesterone levels.
On the hormonal end, endometriosis is always linked to oestrogen dominance. Eating an abundance of green cruciferous vegetables and taking Happy DIM will ensure that your oestrogen is being metabolised well. Additionally, Happy Hormones will help with the communication between your brain and your ovaries to balance hormone production, stimulate proper ovulation and, in turn, increase natural progesterone levels. Ensure you’re managing stress effectively and getting good quality sleep as well.
In essence, endometriosis is so much more than a condition caused by oestrogen dominance. There are many drivers as well as many hypothesised causative factors. A treatment approach which takes these multiple factors into consideration is ideal. If you’re just trying to get by and resorting to using only synthetic hormones which mask your symptoms, you are not treating the underlying cause.
For the best outcome, make sure you’re addressing the following aspects of endometriosis: hormonal, immune, microbial, and digestive. Better yet, take our FREE Hormonal Assessment so you can start off on the right path to healing and wellness!
REFERENCES:
Porpora M, Brunelli R, Costa G, et al. A promise in the treatment of endometriosis: an observational cohort study on ovarian endometrioma reduction by N-acetylcysteine. Evidence-Based Complementary and Alternative Medicine. 2013; April.
https://pubmed.ncbi.nlm.nih.gov/23737821/
Libo Zhu, Xinmei Zhang.[Research advances on the role of mast cells in pelvic pain of endometriosis].Journal of Zhejiang University. Medical Sciences, 01 Jul 2013, 42(4):461-463.
https://pubmed.ncbi.nlm.nih.gov/24022937/
Tian-Hong Zhu, Gen Zou, et. al. Mast cell stabilizer ketotifen reduces hyperalgesia in a rodent model of surgically induced endometriosis. Journal of Pain Research. 2019 Apr 29;12:1359-1369.
https://pubmed.ncbi.nlm.nih.gov/31118754/
Quaranta G, Sanguinetti M, and Masucci L. Fecal Microbiota Transplantation: A Potential Tool for Treatment of Human Female Reproductive Tract Diseases. Frontiers in Immunology. 2019 Nov 26;10:2653. https://pubmed.ncbi.nlm.nih.gov/31827467/
Anderson G. Endometriosis Pathoetiology and Pathophysiology: Roles of Vitamin A, Estrogen, Immunity, Adipocytes, Gut Microbiome and Melatonergic Pathway on Mitochondria Regulation. Biomol Concepts. 2019 Jul 19;10(1):133-149.
https://pubmed.ncbi.nlm.nih.gov/31339848/
Patel B, Rudnicki M, et al. Progesterone resistance in endometriosis: origins, consequences and interventions. Acta Obstetricia et Gynecologica Scandinavica. 2017 Jun;96(6):623-632. https://pubmed.ncbi.nlm.nih.gov/28423456/
Parazzini F, Viganò P, Candiani M, Fedele L. Diet and endometriosis risk: a literature review. Reprod Biomed Online. 2013 Apr;26(4):323-36. https://pubmed.ncbi.nlm.nih.gov/23419794/